What Is Glaucoma?
Glaucoma is a disease that damages your eye's optic nerve. It usually happens when fluid builds up in the front part of your eye. That extra fluid increases the pressure in your eye, damaging the optic nerve.
Glaucoma is a leading cause of blindness for people over 60 years old. But blindness from glaucoma can often be prevented with early treatment. When glaucoma develops, usually you don’t have any early symptoms and the disease progresses slowly. In this way, glaucoma can steal your sight very gradually. Fortunately, early detection and treatment (with glaucoma eye drops, glaucoma surgery or both) can help preserve your vision.
Glaucoma is a disease that damages your eye's optic nerve. It usually happens when fluid builds up in the front part of your eye. That extra fluid increases the pressure in your eye, damaging the optic nerve.
Glaucoma is a leading cause of blindness for people over 60 years old. But blindness from glaucoma can often be prevented with early treatment. When glaucoma develops, usually you don’t have any early symptoms and the disease progresses slowly. In this way, glaucoma can steal your sight very gradually. Fortunately, early detection and treatment (with glaucoma eye drops, glaucoma surgery or both) can help preserve your vision.
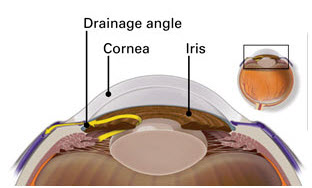
In a healthy eye, excess fluid leaves the eye through the drainage angle, keeping pressure stable.
The optic nerve is connected to the retina — a layer of light-sensitive tissue lining the inside of the eye — and is made up of many nerve fibers, like an electric cable is made up of many wires. The optic nerve sends signals from your retina to your brain, where these signals are interpreted as the images you see.
In the healthy eye, a clear fluid called aqueous (pronounced AY-kwee-us) humor circulates inside the front portion of your eye. To maintain a constant healthy eye pressure, your eye continually produces a small amount of aqueous humor while an equal amount of this fluid flows out of your eye. If you have glaucoma, the aqueous humor does not flow out of the eye properly. Fluid pressure in the eye builds up and, over time, causes damage to the optic nerve fibers.
There are several types of glaucoma:
o Open-angle glaucoma
o Normal-tension glaucoma
o Angle-closure glaucoma (also called "closed-angle glaucoma" or "narrow-angle glaucoma")
o Congenital glaucoma
o Secondary glaucoma
o Glaucoma suspect
Open-angle glaucoma
The most common form of glaucoma is called primary open-angle glaucoma. It occurs when the trabecular meshwork of the eye gradually becomes less efficient at draining fluid. As this happens, your eye pressure, called intraocular pressure (IOP), rises. Raised eye pressure leads to damage of the optic nerve. Damage to the optic nerve can occur at different eye pressures in different patients. There is not one ‘right’ eye pressure that is the same for everyone. Your ophthalmologist establishes a target eye pressure for you that he or she predicts will protect your optic nerve from further damage. Different patients have different target pressures.
Typically, open-angle glaucoma has no symptoms in its early stages and your vision remains normal. As the optic nerve becomes more damaged, blank spots begin to appear in your field of vision. You usually won’t notice these blank spots in your day-to-day activities until the optic nerve is significantly damaged and these spots become large. If all of the optic nerve fibers die, you will be blind.
Half of patients with glaucoma do not have high eye pressure when first examined. Eye pressure is not always the same – it rises and falls from day to day and hour to hour. So a single eye pressure test will miss many people who have glaucoma. In addition to routine eye pressure testing, it is essential that the optic nerve be examined by an ophthalmologist for proper diagnosis.
Normal-tension glaucoma
Although "normal" eye pressure is considered a measurement less than 21 mmHg, this can be misleading. Some people have a type of glaucoma called normal-tension, or low-tension glaucoma. Their eye pressure is consistently below 21 mmHg, but optic nerve damage and loss of vision still occur. People with normal-tension glaucoma are usually treated in the same way as people who have open-angle glaucoma.
Angle-closure glaucoma (also called "closed-angle glaucoma" or "narrow-angle glaucoma")
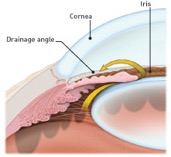
This type happens when someone’s iris is very close to the drainage angle in their eye. The iris can end up blocking the drainage angle. You can think of it like a piece of paper sliding over a sink drain. When the drainage angle gets completely blocked, eye pressure rises very quickly. This is called an acute attack. It is a true eye emergency, and you should call your ophthalmologist right away or you might go blind. People of Asian descent and those with hyperopia (farsightedness) tend to be more at risk for developing this form of glaucoma.
Symptoms of an acute attack include:
o Your vision is suddenly blurry
o severe eye pain
o headache
o feel sick to your stomach (nausea)
o throw up (vomit)
o see rainbow-colored rings or halos around lights
A closed-angle glaucoma attack is a medical emergency and must be treated immediately. Unfortunately, people at risk for developing closed-angle glaucoma often have few or no symptoms before the attack.
People at risk for closed-angle glaucoma should avoid over-the-counter decongestants and other medications where the packaging states not to use these products if you have glaucoma. These products are usually safe to use once your narrow angle has been treated with laser iridotomy. Always ask your ophthalmologist if it is safe for you to use products with this warning.
Congenital glaucoma
Congenital glaucoma is a rare type of glaucoma that develops in infants and young children and can be inherited. While less common than the other types of glaucoma, this condition can be devastating, often resulting in blindness if not diagnosed and treated early.
Secondary glaucoma
Secondary glaucoma is glaucoma that results from another eye condition or disease. For example, someone who has had an eye injury, someone who is on long-term steroid therapy or someone who has a tumor may develop secondary glaucoma. The most common forms of secondary glaucoma are: pseudoexfoliative glaucoma, pigmentary glaucoma, and neovascular glaucoma.
Glaucoma suspect
Some people have normal eye pressure but their optic nerve or visual field looks suspicious for glaucoma. These people must be watched carefully because some eventually develop definite glaucoma and need treatment.
Other people have an eye pressure that is higher than normal, but they do not have other signs of glaucoma, such as optic nerve damage or blank spots that show up in their peripheral (side) vision when tested. This condition is called ocular hypertension. Individuals with ocular hypertension are at higher risk for developing glaucoma compared to people with lower, or average, eye pressure. Just like people with glaucoma, people with ocular hypertension need to be closely monitored by an ophthalmologist to ensure they receive appropriate treatment.
Causes of Glaucoma
Glaucoma causes include elevated eye pressure (called intraocular pressure or IOP) due to the eye’s inability to drain fluid efficiently.
A clear fluid called aqueous humor circulates inside the front portion of our eyes. To maintain a constant healthy eye pressure, the eye continually produces a small amount of aqueous humor while an equal amount of this fluid flows out of the eye. The fluid flows out through a very tiny drain called the trabecular meshwork, a complex network of cells and tissue in an area called the drainage angle.
If the drainage angle is blocked, excess fluid cannot flow out of the eye, causing the fluid pressure to increase.
If you have glaucoma, the aqueous humor does not flow through the trabecular meshwork properly. If the drainage angle is becoming less efficient at draining fluid, as in the common open-angle glaucoma, excess fluid cannot flow out of the eye properly, causing the intraocular pressure (IOP) to increase. Over time, raised IOP causes damage to the nerve fibers. If the drainage angle becomes completely blocked, eye pressure rises quickly, resulting in a narrow-angle glaucoma or angle-closure glaucoma attack, with severe eye and brow pain, nausea and vomiting. This kind of glaucoma attack is a medical emergency and must be treated immediately.
Damage to the optic nerve can occur at different eye pressures among different patients. Your ophthalmologist establishes a target eye pressure for you that he or she predicts will protect your optic nerve from further damage. Different patients have different target pressures.
Some people have a type of glaucoma called normal tension, or low tension glaucoma. Their eye pressure is consistently below 21 mmHg, but optic nerve damage and visual field loss still occur.
Glaucoma can often be caused by another eye condition or disease. This is known as secondary glaucoma. For example, someone who has a tumor or people undergoing long-term steroid therapy may develop secondary glaucoma. Other causes of secondary glaucoma include:
o Eye injury;
o Inflammation of the eye;
o Abnormal blood vessel formation from diabetes or retinal blood vessel blockage;
o Use of steroid-containing medications (pills, eye drops, sprays); or
o Pigment dispersion, where tiny fragments or granules from the iris (the colored part of the eye) can circulate in the aqueous humor (the fluid within the front portion of the eye) and block the trabecular meshwork, the tiny drain for the eye’s aqueous humor.
If you have received glaucoma diagnosis from your Eye M.D., your doctor will talk about possible treatment options, such as glaucoma eye drops and/or glaucoma surgery.
Who Is at Risk for Glaucoma?
Some people are at greater risk for developing glaucoma and should see their ophthalmologist on a regular basis, specifically for glaucoma testing.
People with more risk of developing glaucoma include people who:
o are over age 40;
o have family members with glaucoma;
o are of African or Hispanic heritage;
o are of Asian heritage (Asians are at increased risk of angle closure glaucoma and Japanese are at increased risk of low tension glaucoma);
o have high eye pressure;
o are farsighted or nearsighted;
o have had an eye injury;
o have corneas that are thin in the center; or
o have diabetes, migraines, high blood pressure, poor blood circulation or other health problems affecting the whole body.
Talk with an ophthalmologist about your risk for getting glaucoma. People with more than one of these risk factors have an even higher risk of glaucoma.
Early detection and treatment can protect your vision.
People of any age with glaucoma symptoms or glaucoma risk factors, such as those with diabetes, a family history of glaucoma, or those of African descent, should see an ophthalmologist for an exam. Your ophthalmologist will let you know how often to return for follow-up exams.
Adults with no symptoms of or risk factors for eye disease should have a complete eye disease screening by age 40 — the time when early signs of disease and changes in vision may start to happen. Based on the results of the initial screening, your ophthalmologist will let you know how often to return for follow-up exams.
Adults 65 or older should have an eye exam every one to two years, or as recommended by your ophthalmologist.
People of Asian descent and those with hyperopia (farsightedness) tend to be more at risk for narrow-angle glaucoma (also known as angle-closure glaucoma or closed-angle glaucoma).
If you have received glaucoma diagnosis from your Eye M.D., your doctor will talk about possible treatment options, such as glaucoma eye drops and/or glaucoma surgery.
Diagnosis
The only sure way to diagnose glaucoma is with a complete eye exam. A glaucoma screening that only checks eye pressure is not enough to find glaucoma.
One of the problems with glaucoma, especially open-angle glaucoma, is that there are typically no symptoms in the early stages. Many people who have the disease do not know they have it. This is why it is important, especially as you get older, to have regular medical eye exams by an Eye M.D.
Treatment
How your glaucoma is treated will depend on your specific type of glaucoma, the severity of your disease and how well it responds to treatment.
Glaucoma damage is permanent—it cannot be reversed. But medicine and surgery help to stop further damage. To treat glaucoma, your ophthalmologist may use one or more of the following treatments.
Medication
Medicated eye drops are the most common way to treat glaucoma. These medications lower your eye pressure in one of two ways — either by reducing the amount of fluid created in the eye or by helping this fluid flow out of the eye through the drainage angle.
These eye drops must be taken every day. Just like any other medication, it is important to take your eye drops regularly as prescribed by your ophthalmologist.
Once you are taking medications for glaucoma, your ophthalmologist will want to see you regularly. You can expect to visit your ophthalmologist about every 3–6 months. However, this can vary depending on your treatment needs.
Laser trabeculoplasty
A surgery called laser trabeculoplasty is often used to treat open-angle glaucoma. There are two types of trabeculoplasty surgery: argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT).
Damage to the optic nerve can occur at different eye pressures among different patients. Your ophthalmologist establishes a target eye pressure for you that he or she predicts will protect your optic nerve from further damage. Different patients have different target pressures.
Some people have a type of glaucoma called normal tension, or low tension glaucoma. Their eye pressure is consistently below 21 mmHg, but optic nerve damage and visual field loss still occur.
Glaucoma can often be caused by another eye condition or disease. This is known as secondary glaucoma. For example, someone who has a tumor or people undergoing long-term steroid therapy may develop secondary glaucoma. Other causes of secondary glaucoma include:
o Eye injury;
o Inflammation of the eye;
o Abnormal blood vessel formation from diabetes or retinal blood vessel blockage;
o Use of steroid-containing medications (pills, eye drops, sprays); or
o Pigment dispersion, where tiny fragments or granules from the iris (the colored part of the eye) can circulate in the aqueous humor (the fluid within the front portion of the eye) and block the trabecular meshwork, the tiny drain for the eye’s aqueous humor.
If you have received glaucoma diagnosis from your Eye M.D., your doctor will talk about possible treatment options, such as glaucoma eye drops and/or glaucoma surgery.
Who Is at Risk for Glaucoma?
Some people are at greater risk for developing glaucoma and should see their ophthalmologist on a regular basis, specifically for glaucoma testing.
People with more risk of developing glaucoma include people who:
o are over age 40;
o have family members with glaucoma;
o are of African or Hispanic heritage;
o are of Asian heritage (Asians are at increased risk of angle closure glaucoma and Japanese are at increased risk of low tension glaucoma);
o have high eye pressure;
o are farsighted or nearsighted;
o have had an eye injury;
o have corneas that are thin in the center; or
o have diabetes, migraines, high blood pressure, poor blood circulation or other health problems affecting the whole body.
Talk with an ophthalmologist about your risk for getting glaucoma. People with more than one of these risk factors have an even higher risk of glaucoma.
Early detection and treatment can protect your vision.
People of any age with glaucoma symptoms or glaucoma risk factors, such as those with diabetes, a family history of glaucoma, or those of African descent, should see an ophthalmologist for an exam. Your ophthalmologist will let you know how often to return for follow-up exams.
Adults with no symptoms of or risk factors for eye disease should have a complete eye disease screening by age 40 — the time when early signs of disease and changes in vision may start to happen. Based on the results of the initial screening, your ophthalmologist will let you know how often to return for follow-up exams.
Adults 65 or older should have an eye exam every one to two years, or as recommended by your ophthalmologist.
People of Asian descent and those with hyperopia (farsightedness) tend to be more at risk for narrow-angle glaucoma (also known as angle-closure glaucoma or closed-angle glaucoma).
If you have received glaucoma diagnosis from your Eye M.D., your doctor will talk about possible treatment options, such as glaucoma eye drops and/or glaucoma surgery.
Diagnosis
The only sure way to diagnose glaucoma is with a complete eye exam. A glaucoma screening that only checks eye pressure is not enough to find glaucoma.
One of the problems with glaucoma, especially open-angle glaucoma, is that there are typically no symptoms in the early stages. Many people who have the disease do not know they have it. This is why it is important, especially as you get older, to have regular medical eye exams by an Eye M.D.
Treatment
How your glaucoma is treated will depend on your specific type of glaucoma, the severity of your disease and how well it responds to treatment.
Glaucoma damage is permanent—it cannot be reversed. But medicine and surgery help to stop further damage. To treat glaucoma, your ophthalmologist may use one or more of the following treatments.
Medication
Medicated eye drops are the most common way to treat glaucoma. These medications lower your eye pressure in one of two ways — either by reducing the amount of fluid created in the eye or by helping this fluid flow out of the eye through the drainage angle.
These eye drops must be taken every day. Just like any other medication, it is important to take your eye drops regularly as prescribed by your ophthalmologist.
Once you are taking medications for glaucoma, your ophthalmologist will want to see you regularly. You can expect to visit your ophthalmologist about every 3–6 months. However, this can vary depending on your treatment needs.
Laser trabeculoplasty
A surgery called laser trabeculoplasty is often used to treat open-angle glaucoma. There are two types of trabeculoplasty surgery: argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT).
During ALT surgery, a laser makes tiny, evenly spaced burns in the trabecular meshwork. The laser does not create new drainage holes, but rather stimulates the drain to work better.
SLT uses a newer, lower-energy laser which only treats specific cells in the drainage angle. SLT and ALT are equally good at lowering eye pressure.
SLT uses a newer, lower-energy laser which only treats specific cells in the drainage angle. SLT and ALT are equally good at lowering eye pressure.
Even if laser trabeculoplasty is successful, most patients continue taking glaucoma medications after surgery. For many, this surgery is not a permanent solution. Nearly half of the people who receive this surgery develop increased eye pressure again within five years. Many people who have had a successful laser trabeculoplasty will need more treatment in the future. This treatment may be another laser, more medication or surgery.
Laser trabeculoplasty can also be used as a first line of treatment for patients who are unwilling or unable to use glaucoma eye drops.
Laser iridotomy
Laser iridotomy is recommended for treating people with closed-angle glaucoma and those with very narrow drainage angles. A laser creates a small hole about the size of a pinhead through the iris to improve the flow of aqueous fluid to the drainage angle.
Peripheral iridectomy
When laser iridotomy is unable to stop an acute closed-angle glaucoma attack, or is not possible for other reasons, a peripheral iridectomy may be performed. This is performed in an operating room. A small piece of the iris is removed, giving the aqueous fluid access to the drainage angle again. Because most cases of closed-angle glaucoma can be treated with glaucoma medications and laser iridotomy, peripheral iridectomy is rarely necessary.
Laser trabeculoplasty can also be used as a first line of treatment for patients who are unwilling or unable to use glaucoma eye drops.
Laser iridotomy
Laser iridotomy is recommended for treating people with closed-angle glaucoma and those with very narrow drainage angles. A laser creates a small hole about the size of a pinhead through the iris to improve the flow of aqueous fluid to the drainage angle.
Peripheral iridectomy
When laser iridotomy is unable to stop an acute closed-angle glaucoma attack, or is not possible for other reasons, a peripheral iridectomy may be performed. This is performed in an operating room. A small piece of the iris is removed, giving the aqueous fluid access to the drainage angle again. Because most cases of closed-angle glaucoma can be treated with glaucoma medications and laser iridotomy, peripheral iridectomy is rarely necessary.

In trabeculectomy, a flap is first created in the sclera (the white part of the eye). Then a small opening is made into the eye to release fluid from the eye.
Trabeculectomy
In trabeculectomy, a small flap is made in the sclera (the outer white coating of your eye). A filtration bleb, or reservoir, is created under the conjunctiva — the thin, filmy membrane that covers the white part of your eye. Once created, the bleb looks like a bump or blister on the white part of the eye above the iris, but the upper eyelid usually covers it. The aqueous humor can now drain through the flap made in the sclera and collect in the bleb, where the fluid will be absorbed into blood vessels around the eye.
Eye pressure is effectively controlled in three out of four people who have trabeculectomy. Although regular follow-up visits with your doctor are still necessary, many patients no longer need to use eye drops. If the new drainage channel closes or too much fluid begins to drain from the eye, additional surgery may be needed.
Aqueous shunt surgery
If trabeculectomy cannot be performed, aqueous shunt surgery is usually successful in lowering eye pressure.
In trabeculectomy, a small flap is made in the sclera (the outer white coating of your eye). A filtration bleb, or reservoir, is created under the conjunctiva — the thin, filmy membrane that covers the white part of your eye. Once created, the bleb looks like a bump or blister on the white part of the eye above the iris, but the upper eyelid usually covers it. The aqueous humor can now drain through the flap made in the sclera and collect in the bleb, where the fluid will be absorbed into blood vessels around the eye.
Eye pressure is effectively controlled in three out of four people who have trabeculectomy. Although regular follow-up visits with your doctor are still necessary, many patients no longer need to use eye drops. If the new drainage channel closes or too much fluid begins to drain from the eye, additional surgery may be needed.
Aqueous shunt surgery
If trabeculectomy cannot be performed, aqueous shunt surgery is usually successful in lowering eye pressure.
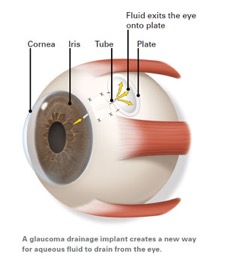
An aqueous shunt, or glaucoma drainage device, is a small plastic tube or valve connected to a reservoir (a roundish or oval plate). The plate is placed on the outside of the eye beneath the conjunctiva (the thin membrane that covers the inside of your eyelids and the white part of your eye). The tube is placed into the eye through a tiny incision and allows aqueous humor to flow through the tube to the plate. The fluid is then absorbed into the blood vessels. When healed, the reservoir is not easily seen unless you look downward and lift your eyelid.
Important things to remember about glaucoma treatment
There are a number of ways to treat glaucoma. While some people may experience side effects from glaucoma medications or glaucoma surgery, the risks of side effects should always be balanced with the greater risk of leaving glaucoma untreated and losing vision.
If you have glaucoma, preserving your vision requires strong teamwork between you and your doctor. Your doctor can prescribe treatment, but it’s important to do your part by following your treatment plan closely. Be sure to take your medications as prescribed and see your ophthalmologist regularly.
by www.aao.org
Important things to remember about glaucoma treatment
There are a number of ways to treat glaucoma. While some people may experience side effects from glaucoma medications or glaucoma surgery, the risks of side effects should always be balanced with the greater risk of leaving glaucoma untreated and losing vision.
If you have glaucoma, preserving your vision requires strong teamwork between you and your doctor. Your doctor can prescribe treatment, but it’s important to do your part by following your treatment plan closely. Be sure to take your medications as prescribed and see your ophthalmologist regularly.
by www.aao.org
Cr. Picture : https://www.healingtheeye.com ิ
 02-056-3333
02-056-3333