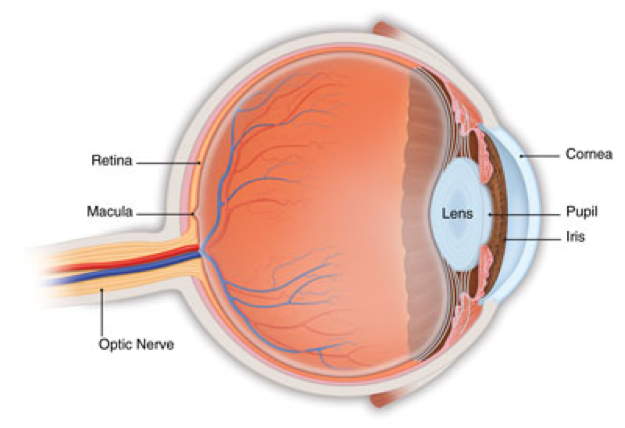
Age-related macular degeneration (AMD) is a deterioration or breakdown of the eye's macula. The macula is a small area in the retina — the light-sensitive tissue lining the back of the eye. The macula is the part of the retina that is responsible for your central vision, allowing you to see fine details clearly.
The macula makes up only a small part of the retina, yet it is much more sensitive to detail than the rest of the retina (called the peripheral retina). The macula is what allows you to thread a needle, read small print, and read street signs. The peripheral retina gives you side (or peripheral) vision. If someone is standing off to one side of your vision, your peripheral retina helps you know that person is there by allowing you to see their general shape.
Many older people develop macular degeneration as part of the body's natural aging process.
There are different kinds of macular problems, but the most common is age-related macular degeneration.
Types of macular degeneration
Dry macular degeneration and Wet macular degeneration
There are two types of macular degeneration:
Dry, or atrophic, macular degeneration (also called non-neovascular macular degeneration) with drusen
Most people who have macular degeneration have the dry form. This condition is caused by aging and thinning of the tissues of the macula. Macular degeneration usually begins when tiny yellow or white pieces of fatty protein called drusen form under the retina. Eventually, the macula may become thinner and stop working properly. With dry macular degeneration, vision loss is usually gradual. People who develop dry macular degeneration must carefully and constantly monitor their central vision. If you notice any changes in your vision, you should tell your ophthalmologistright away, as the dry form can change into the more damaging form of macular degeneration called wet (exudative) macular degeneration. While there is no medication or treatment for dry macular degeneration, some people may benefit from a vitamin therapy regimen for dry macular degeneration.
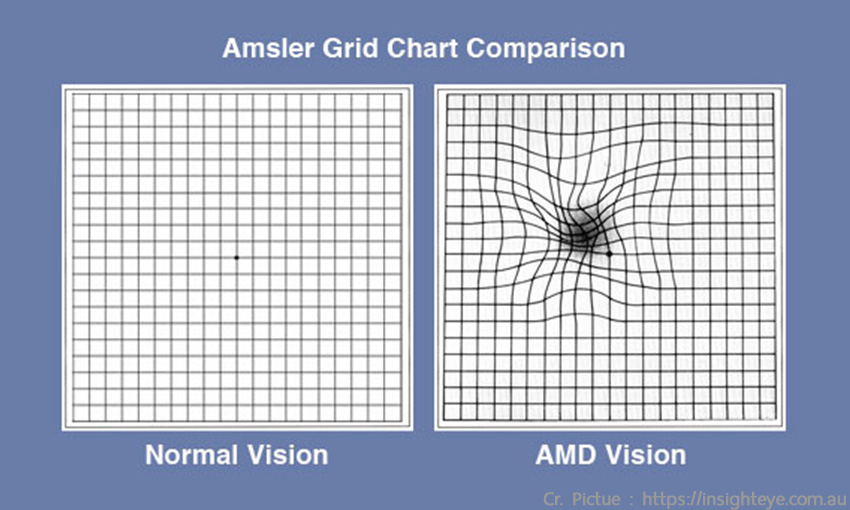
Using an Amsler grid to test for macular degeneration
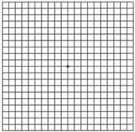
If you have been diagnosed with dry macular degeneration, you should use a chart called an Amsler grid every day to monitor your vision, as dry macular degeneration can change into the more damaging wet form.
To use the Amsler grid, wear your reading glasses and hold the grid 12 to 15 inches away from your face in good light.
o Cover one eye.
o Look directly at the center dot with the uncovered eye and keep your eye focused on it.
o While looking directly at the center dot, note whether all lines of the grid are straight or if any areas are distorted, blurry or dark.
o Repeat this procedure with the other eye.
o If any area of the grid looks wavy, blurred or dark, contact your ophthalmologist.
o If you detect any changes when looking at the grid, you should notify your ophthalmologist immediately.
Wet, or exudative, macular degeneration (also called neovascular macular degeneration)
About 10 percent of people who have macular degeneration have the wet form, but it can cause more damage to your central or detail vision than the dry form. Wet macular degeneration occurs when abnormal blood vessels begin to grow underneath the retina. This blood vessel growth is called choroidal neovascularization (CNV) because these vessels grow from the layer under the retina called the choroid. These new blood vessels may leak fluid or blood, blurring or distorting central vision. Vision loss from this form of macular degeneration may be faster and more noticeable than that from dry macular degeneration.
The longer these abnormal vessels leak or grow, the more risk you have of losing more of your detailed vision. Also, if abnormal blood vessel growth happens in one eye, there is a risk that it will occur in the other eye. The earlier that wet macular degeneration is diagnosed and treated, the better chance you have of preserving some or much of your central vision. That is why it is so important that you and your ophthalmologist monitor your vision in each eye carefully.
Dry macular degeneration signs and symptoms
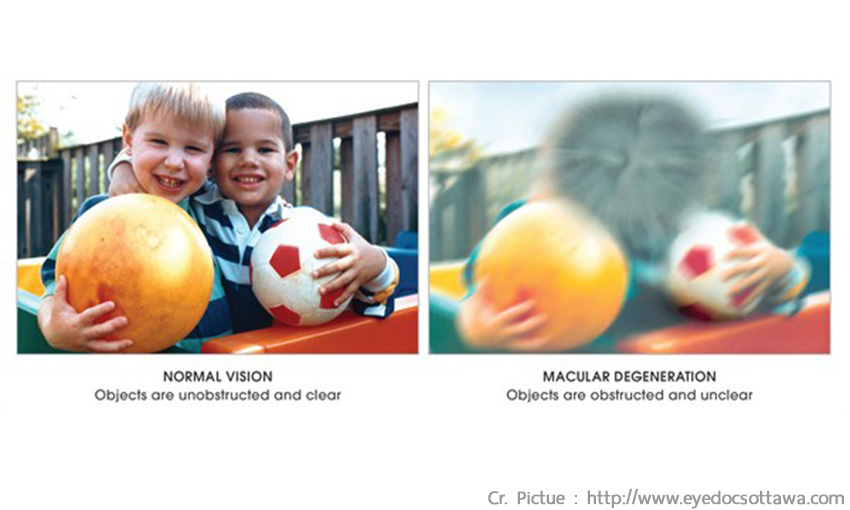
o Blurry distance and/or reading vision
o Need for increasingly bright light to see up close
o Colors appear less vivid or bright
o Hazy vision
o Difficulty seeing when going from bright light to low light (such as entering a dimly lit room from the bright outdoors)
o Trouble or inability to recognize people's faces
o Blank or blurry spot in your central vision
Dry macular degeneration can affect one or both eyes. You may not notice vision changes if only one eye is affected, as your unaffected eye will compensate for vision loss in the other eye.
Wet macular degeneration signs and symptoms
o Distorted vision — straight lines will appear bent, crooked or irregular
o Dark gray spots or blank spots in your vision
o Loss of central vision
o Size of objects may appear different for each eye
o Colors lose their brightness; colors do not look the same for each eyeWet macular degeneration symptoms usually appear and get worse fairly quickly.
Macular Degeneration Treatment
Dry AMD and nutritional supplements
Unfortunately, at this time there is no single proven treatment for the dry form of macular degeneration. However, a large scientific study has shown that antioxidant vitamins and zinc may reduce the impact of macular degeneration in some people by slowing its progression toward more advanced stages.
Wet macular degeneration treatment
Treating the wet form of macular degeneration may involve the use of anti-VEGF treatment, thermal laser treatment or photodynamic therapy (PDT). Treatment of wet macular degeneration generally reduces—but does not eliminate-- the risk of severe vision loss.
1. Anti-VEGF medication injection treatments for wet macular degeneration
A common way to treat wet macular degeneration targets a specific chemical in your body that causes abnormal blood vessels to grow under the retina. That chemical is called vascular endothelial growth factor, or VEGF. Several new drug treatments (called anti-VEGF drugs) have been developed for wet AMD that can block the trouble-causing VEGF. Blocking VEGF reduces the growth of abnormal blood vessels, slows their leakage, helps to slow vision loss, and in some cases improves vision.
Your ophthalmologist administers the anti-VEGF drug (such as Avastin, Lucentis, and Eylea) directly to your eye in an outpatient procedure. Before the procedure, your ophthalmologist will clean your eye to prevent infection and will use an anesthetic drop or injection of anesthetic with a very fine needle to numb your eye. You may receive multiple anti-VEGF injections over the course of many months. Repeat anti-VEGF treatments are often needed for continued benefit.
In some cases, your ophthalmologist may recommend combining anti-VEGF treatment with other therapies. The treatment that’s right for you will depend on the specific condition of your macular degeneration.
2. Laser treatment for wet macular degeneration
Although most cases of wet AMD are treated with medication, in some instances thermal laser therapy may be used. Laser treatment is usually done as an outpatient procedure in the doctor’s office or at the hospital. The laser beam in this procedure is a high-energy, focused beam of light that produces a small burn when it hits the area of the retina to be treated. This destroys the abnormal blood vessels, preventing further leakage, bleeding and growth. Following laser treatment, vision may be more blurred than before treatment, but often it will stabilize within a few weeks. A scar forms where the treatment occurred, creating a permanent blind spot that might be noticeable in your field of vision.
Usually the abnormal blood vessels are destroyed by laser treatment. However, it is likely that 50 percent of patients with wet macular degeneration who receive this laser procedure will need a re-treatment within three to five years. You may be instructed to use the Amsler grid daily to monitor your vision for signs of change.
3.Photodynamic therapy (PDT)
In some cases, a type of treatment for wet macular degeneration called photodynamic therapy, or PDT, may be an option. This therapy uses a combination of a light-activated drug called a photosensitizer and a special low-power, or cool, laser to treat wet macular degeneration right at the center of the macula. This procedure is done on an outpatient basis, usually in an ophthalmologist’s office. The photosensitive drug is injected into a vein in your arm, where it travels through the body, including the abnormal vessels behind the central macula. The low-power laser light is targeted directly on the abnormal vessels, activating the drug, which causes damage specifically to those unwanted blood vessels. After PDT, the abnormal blood vessels may reopen, so multiple treatments may be required.
by www.aao.org
 02-056-3333
02-056-3333